The world has been brought to its knees by a virus. Which begs the question:
What’s a virus?
If you are not exactly sure, you are not alone.
We all know we need to avoid “Germs” because they can make us sick, but there are two kinds of germs: Bacteria and Viruses (Actually there are 4– I am ignoring fungi and protozoa.)
The confusion between bacteria & viruses is common. One study showed 41% of Americans think antibiotics can treat a virus, including the flu (35%) or a common cold (24%). (The same poll in Britain showed about the same numbers, Australians were much more confused.)
Something tiny (500 million rhinoviruses -which cause the common cold- could fit on to the head of a pin) has America, “The World’s Most Powerful Country” locked indoors this summer.
I thought a review of basic information might help- or at least fill a few more minutes of quarantine.
Viruses and Bacteria are different Animals
I say “Animals” in jest- in fact calling a Virus a “living thing” is controversial.
Bacteria are one-cell organisms that can live independently (within limits, of course), whereas viruses are “just capsules that contain genetic material” [quote]. Viruses do not include all the biochemical processes necessary to survive and, therefore, must co-opt the functions of the cell they invade (the “Host Cell”). The Viral hijacker makes the Host Cell do its bidding. [source]
The size and complexity of bacteria and viruses are dramatically different, but I think both have an inherent beauty. You don’t believe me? Take a moment to inspect some good looking bacteria and viruses of various shapes and sizes. Better yet- here are some COVID-19 paintings my artist sister Amanda Wicks Freymann created as she was learning to cope with quarantine this March:


Viruses vs. Bacteria: How can you tell?
Both bacteria and viruses cause infections, and some conditions have two possible sources (bacterial pneumonia vs. viral pneumonia, bacterial meningitis vs. viral meningitis).
A person sick with either a virus or bacteria can have similar symptoms because the immune system attacks both with the same tactics. Coughing, sneezing, fever, inflammation, vomiting, diarrhea, and muscle fatigue are all common side-effects of the battle raging between the body’s defenses and the invading germ. It can be challenging to determine if a person has a bacterial or viral infection from symptoms alone (and the color of the snot is not the key!)
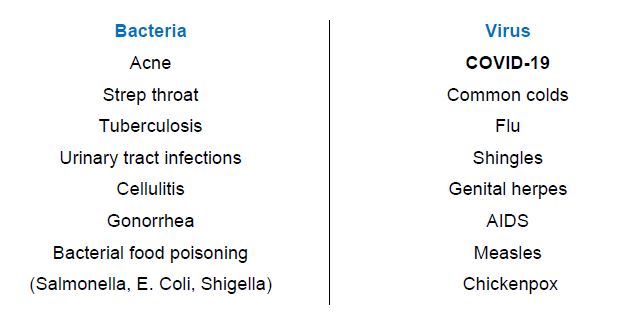
Both Bacterial and Viral infections are well known to us. These are just some:
I discovered two good short films that will help explain the differences between bacterial and viral illnesses: an easy 3-minute review by a physician from Boys Town National Research Hospital (here) and a tremendously entertaining 8 min cartoon (done by a Veterinarian) on Plain and Simple (here).
Treating Infections: Bacteria
We all know about antibiotics; in 2013, the Centers for Disease Control and Prevention [CDC] reported that 4 out of 5 Americans had a prescription.
However, as a country, our antibiotic use is going down [map]:
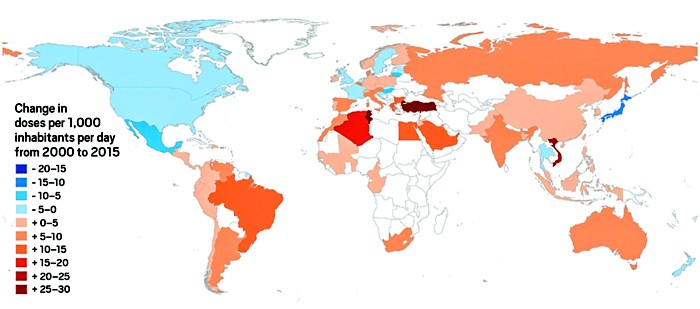
The decrease is in response to the development of antibiotic-resistant “superbugs” and the importance of “Antibiotic Stewardship.” For more, see Fontenotes #58.
Treating Infections: Viruses
Usually viruses take care of themselves. You might feel terrible, but after 3 days to a week, your body will fight it off. This is why treatment options include “managing symptoms, such as honey for coughs and warm fluids like chicken soup for oral hydration.” [quote]
Most medications available to fight viruses (called, not surprisingly, “Antiviral” drugs) only resolve your symptoms, not the infection itself. As an example, if you have the flu, there is a prescription that can decrease your suffering- by one day.
Even the much-touted Antiviral agent Remdesivir only limits the length of COVID-19 (by as much as 4 days) but is not a cure. Decreasing the time may increase a patient’s chance of survival, but it is not the magic bullet the media might have you believe. (For more on Remdesivir, see below.)
Antiviral drugs are only available for only a limited number of infections. One reason is it is difficult to destroy the virus without harming the Host Cell as well. (In contrast, antibiotics kill bacteria, which are “free-standing” so to speak.)
The most successful Antiviral drugs currently available are used to treat infections caused by HIV/AIDS, herpesviruses (including cold sore applications), hepatitis B and C viruses, and influenza A and B.
Without an arsenal of drugs to knock out viruses, the best treatment is to avoid them altogether. And that means being vaccinated.
I know there are “Anti-Vaxers.” For the rest of us, let’s celebrate the 14 “Diseases You Almost Forgot About (Thanks to Vaccines),” including Polio, Tetanus, Measles, Whooping Cough, Mumps, and Diphtheria. The ravages of these diseases across America are as recent as the memories of my parents.
We don’t have vaccines against all viruses- most noticeably AIDS. That is because The HIV virus is “uniquely challenging” in where it attacks (the patient’s own immune system), and HIV mutates rapidly- even within one person. MERS (Middle East Respiratory Syndrome) and SARS (Severe Acute Respiratory Syndrome) are also “fast mutators” that make effective vaccines difficult. Sadly, for some other viruses, the lack of a vaccine reflects the cost of development.
Cost, however, will not be an issue in the development of a vaccine for COVID-19. The Federal Government announced July 7th an investment over 2 Billion dollars, plus another $783 million to three companies to manufacture whichever COVID-19 vaccines get approved by the FDA.
We already see promising signs in that effort. A Phase Three trial started this week, and the results of that trial could be available as soon as November. That may sound like “forever,” but this progress is remarkable! Before now, the fastest development of a vaccine was for Mumps. It took four years.
And what do we do while we wait?
You Know The Drill: Masks! Good Hand Hygiene! & Social Distancing!
I hope understanding why helps the wait.
Want to Know More?
1. In April, Remdesivir was advocated as a treatment for the most severely affected by COVID-19, but those recommendations are changing.
NIH Covid-19 Treatment Guidelines (July 24th) recommend the Antiviral for hospitalized patients requiring supplemental Oxygen (not high-flow or mechanical), with a reduction in the recovery time of up to 4 days, but was of inconclusive benefit for non-hospitalized patients with mild to moderate disease. The sickest patients (those on high flow oxygen, mechanical ventilation, or Extracorporeal membrane oxygenation) showed no observed difference between Remdesivir recipients and patients on a placebo.
The price for Remdesivir was announced on June 29th: for a hospitalized patient with private insurance, the cost will vary between $3,120 and $5,720, depending on the length of treatment. In the meantime, supplies of the drug are low, and some hospitals are running out of the drug.
2. Which country uses the most antibiotics? In 2018 the World Health Organization [WHO] reported on the utilization of antibiotics country-by-country and listed the top 10 offenders– but weirdly (suspiciously?) America, India (named “the world’s biggest consumer of antibiotics” in 2018) and China (which has “a high rate of antibiotic use”) were not included in the survey!