As the Adjunct Professor of Health Law in the Department of Health Care Administration at Trinity University (San Antonio) for the past 22 years, I have always taught my graduate students about the legal issues involving end of life care.
Again this summer, as I looked at my students’ earnest faces, I was reminded of the coma patients I cared for when I was a neurosurgical nurse and just their age. My patients were mostly all in their 20s too.
We all know it is crucial to put in place legal documents that will help if we can’t speak for ourselves about our medical care, but we typically do this when we are in the last third of our life, not the first third.
Young adults need to be planning for the unimaginable as well.
Why are Young Adults at Risk?
There are numerous reasons people could wind up in a situation where they cannot express their wishes regarding medical care- but in this Fontenotes, I am thinking specifically of patients who are in a long-term coma- their lives sustained through artificial nutrition, a respirator, or both.
People may be in a coma- a prolonged state of unconsciousness– because of a stroke, tumor, or other illness- but Traumatic Brain Injury (TBI) is the leading cause.
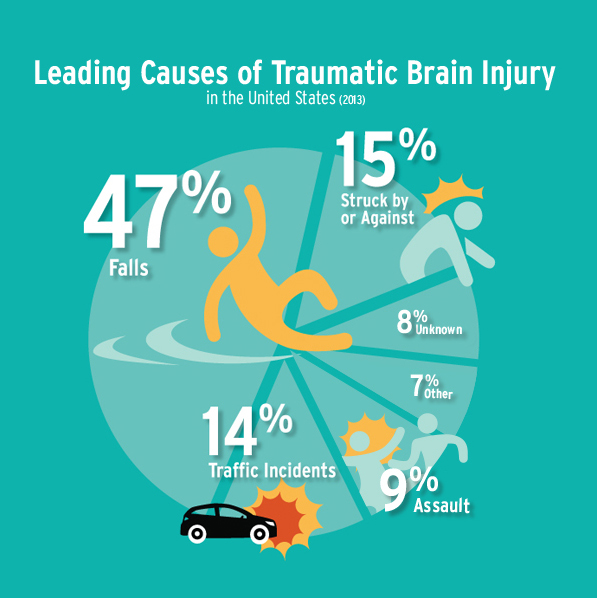
People sustain significant trauma to their brain (TBI) for a variety of reasons- as illustrated by this infographic from brainline:
With the risk of motor vehicle crashes highest for people between the ages of 16 and 19 years old (this population is three-times more likely to be in a fatal crash), the higher incidence of assault and violent crime among young adults, and the prevalence of electronic scooters, bikes, and skateboards as alternative modes of transportation, (often without the protection of a helmet– which cut the incidence of TBI in half in bike accidents)- it is understandable why so many young adults become coma patients.
Calling on healthy young adults to consider writing out their wishes- when long-term coma patients are commonly from that age group- is logical. Unfortunately, only 7% of people between the ages of 18 and 29 have done so.
End of Life Planning for Young Adults
I want to speak directly to those of you who are young adults (or their parents who are reading).
From my own experience, I know that deciding how to care for young people left in a suspended state is one of the most challenging times in health care, but more importantly, a cruel crisis for those patients’ families.
Please understand I am not suggesting that any document or preplanning will diminish the horror if your young life is destroyed by a serious head injury. What I am saying is you should be talking about this when you can. Should the unimaginable happen, at least we will know what you want us to do.
You might be thinking that your State law would help your family if they wanted to decide what to do about your medical care if you were incompetent, and that may be true. And you might be knowledgeable about processes that have been in place for decades that allow loved ones to make tough decisions about life supports under terrible conditions. Those processes might be available to your loved ones too.
But wouldn’t it be better to know there was no question about how to proceed if you were ever in a situation where you could no longer choose for yourself? Wouldn’t you rather decide what you want so you do not put your loved ones in the position of having to speak (and possibly fight) for you?
Does a “Living Will” Mean I Want to Die?
An unfortunate misunderstanding about end of life planning is that most people think a “Living Will” is synonymous with the termination of life supports. Nothing could be further from the truth. The whole point of documenting your wishes is that you are determining your own future. If you only have one option in how you write your directions (cessation of treatment), it isn’t providing you with a choice.
Do you want to be kept alive at all costs? Do you want a feeding tube if you need one, but not a respirator? Would you like to die at home? Do you want to be an organ donor? Most important of all, who do you want to be your legal representative who can speak for you if you can’t speak for yourself? These are the type of decisions you need to make for yourself while you are competent to do so
What Do I Do Next?
- Deciding how you feel about your future if everything goes very badly is the first step of Advanced Care Planning.
- The second step is closely related, and that is to learn about your options to speak for yourself. Fortunately, there are great resources available to you through the American Academy of Pediatrics, the Mayo Clinic, the American Bar Association, as well as your insurance company, state government, and your place of worship. Speaking of which, many of you will want to talk to your pastor, priest, rabbi, imam, or whoever serves as your spiritual guide as part of your end of life decision-making process.
- You now need to document what you want. Think of this as you speaking for yourself in the future (no one can deny your right to do that!) Write out your wishes; hand-written is best (to help prove authorship). There are state-specific suggestions for Living Wills freely available on the web- follow any format your state requires. Your physician’s office, your local hospital, and your public library are also resources for more information on how to draft your directive.
- The last step is to talk to whoever will speak for you when you can’t (your loved ones and whoever you want to designate as your decision-maker). Those you hold closest need to be included in this very private decision of yours.
Sit down with your loved ones and tell them in detail your thoughts about your death and what medical care you want (or not) if you are in a long-term coma.
You also need to talk to your doctor, or whoever your primary care provider is. If they don’t know what you want, it does not make much sense, right? Advanced Life Planning should not be a secret! Give them a copy of your Living Will to be part of your medical record.
But I Don’t Want To
Does this all sound like a lot of time and effort? Do you hate talking about death, dying, and terrible things that could happen? Do you think this is much too serious a conversation to have at this point of time in your life?
I understand but think about the alternative.
Regardless if you want every new technology or comfort care only, your only alternative is to speak for yourself proactively before you reach that point. And that time is now.
Want to Know More?
- For more information about Traumatic Brain Injuries, there is an excellent fact sheet from CDC; and extensive information from the Mayo Clinic– both written for people who do not have medical knowledge (i.e., they are in clear English).
- The Mayo Clinic also has a resource where you can learn more about Coma; if you would like to know about different grades of coma- and how health care professionals determine who is more likely to come out of a coma- you can learn more about the Glasgow Coma Scale from TraumaticBrainInjury.com.